GLIDE Harm Reduction Services director Paul Harkin demystifies fentanyl and shares the known solutions to the opioid crisis
Reprinted from Glide, https://www.glide.org/facts-on-fentanyl/
Friday, August 30, is Overdose Awareness Day, dedicated to remembering lives lost and lives saved in the opioid crisis, as well as to informing the public about humane and evidence-based ways to mitigate the risks and fatalities associated with drug use. Here in the TL, we’ll be gathering from 1:00 to 3:00 pm at the Tenderloin National Forest (511 Ellis Street) to honor the lives lost, as well as to celebrate the power of community—by sharing information, Narcan trainings, our stories, and good food and music. This day and everyday, it’s important to remember that there are things we can all do to reduce risks and harms in our community. The first step is educating ourselves on the facts about drugs and drug use, including the known health interventions out there. Current media attention on fentanyl, a powerful synthetic opioid helping to fuel overdoses in the Bay Area and across the country, is too often inclined to focus on the sensational or to even trade in misinformation. We know that sensationalistic stories only make matters worse. So to learn more about fentanyl and the proven health interventions that can reduce the risks it presents, we spoke with Paul Harkin, director of GLIDE’s HIV/Hep C and Harm Reduction Services. The following conversation has been shortened and lightly edited for clarity.
Can you give us some context for the current focus on fentanyl?
Paul Harkin: I came to San Francisco in 2000 to work at the Tenderloin AIDS Resource Center. My first week at work I saw people who were using fentanyl. Even back then, there were people for whom that was their drug of choice, because it’s fast-acting and it doesn’t last as long. There was not the same hysteria around it then. I just saw it as another opioid among the many opioids that are available to people, whether it’s a pharmaceutical or street drug.
About three years ago, we saw a real uptick in fentanyl in the drug supply in San Francisco. One of the first things we saw was Xanax pills that were counterfeit and had fentanyl. So, you’ve got people that are taking a pill that they thought was a benzodiazepine and it’s full of fentanyl, and they died, or they overdosed.
It was very perplexing. You’re wondering, who would do that? We don’t know if some of this is cross-contamination. There’s been fentanyl traces in a lot of different substances.
And we’re still seeing a lot of opioid users dying from fentanyl overdosing because it’s very strong and the onset is so quick. If I were doing heroin, an overdose is probably about 30 minutes from the shot to the point where I have respiratory failure. There’s quite a decent window there to save me, if there’s anybody around. With fentanyl, that respiratory failure can happen within five minutes.
What’s the approach you and GLIDE take to this situation?
[Fentanyl] has been here for a long time. It’s given to pregnant mothers in maternity wards during childbirth. Any approach that’s hysterical is counterproductive. We just need to look at it rationally: It’s an opioid. It’s a strong opioid. It’s a fast-acting opioid. People have used it for years and not come to harm. Other people have used it once and died. Like with a lot of drugs. We can’t be shaming, stigmatizing, sensationalizing. We just have to educate people that overdoses are reversible. No matter how much somebody takes or how quickly they go into an overdose, if somebody there has Narcan they’re going to be able to reverse that overdose. That means we need to have Narcan distribution.
But we also have to create a climate where people are not using alone, because then nobody can reverse your overdose. It’s like having a designated driver, having somebody with you when you get high. For some folks that’s a challenge because they don’t want to be outed—they might be using drugs secretly. That’s an ongoing community intervention, trying to de-stigmatize use so that people can feel safe to have somebody with them.
Can you elaborate on the life-threatening consequences associated with stigma?
When we look at stigma, whether it’s drug use or sexual behaviors, it’s always been counterproductive. It makes people want to keep secrets; it pushes people further away. By de-stigmatizing substances and substance use you make it easier for someone to talk about it. You can check in with them. “Hey, I’ve noticed you’re getting high a lot more lately. What’s going on? Is everything OK?” You can have that conversation. That’s what we have to get to.
It’s just like with gay men and HIV. We saw that stigma helped promote the infection, because people were feeling unable to discuss their status or getting tested—there was shame, there was stigma, there was criminalization. All of these things are counterproductive. We need to move away from that model. People need the facts, told in a calm and composed way. And then we work with them, based on the facts, on how to reduce the harms.
What are the known health interventions that can reduce or eliminate the threat of overdose deaths?
When we talk about the shocking uptick in opioid overdoses, we should also be talking about the known solutions.
Number one is having overdose prevention available to you through Narcan. If everyone who used had somebody sitting there with Narcan there would be no more overdoses.
Another intervention would be having safe consumption sites where people are medically supervised, or they’re supervised by community members trained in overdose prevention. We have these all over the world. There’s never been a single overdose death in any of them.
Another intervention that we use at GLIDE is giving people fentanyl test strips. It’s not sufficiently adequate because it’s just saying, yes, there is fentanyl in this drug. It’s not telling you the degree of contamination, the percentage of the drug that is fentanyl. However, if you bought ecstasy and it tested positive for fentanyl then that’s a big deal. Now, if you’re buying heroin and it tested positive for fentanyl, that’s also a big deal but it’s still in the same class of drug. So maybe you take less of it. You do a test shot, or you smoke a bit. There are different tried and tested methods that reduce the possibility of overdose.
With those test strips, another good thing about them is that they help us generate conversations about overdose and make sure that people are very aware of how strong fentanyl is and the uptick in the incidences of overdoses, including fatal overdoses.
But, to me, we’re not going to get beyond the opioid deaths until we get to safe consumption sites. There’s really no downside, except for people who see it as a moral failing and they’re morally outraged. It’s coming from an ill-informed position. Let’s talk to drug users, and let’s talk to people who work with drug users and have expertise. You’ll see that the evidence shows that this is a highly efficacious intervention.
It’s like people who say our thoughts and prayers are with you after mass shootings, but they don’t want to touch gun legislation—saying you’re outraged at the opioid crisis and all these deaths, but you won’t implement evidence-based solutions. It’s really time for the people who work with this population, the medical experts, to say we need to do these interventions. The time has come.
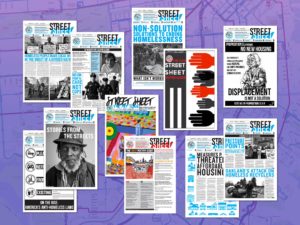
Paul Harkin (above, second from left) is the director of GLIDE’s HIV/Hep C and Harm Reduction Services.